Seeking fitspiration on social media?

Now that it’s 2024, perhaps you’ve thought about taking up a new exercise program, eating better, or some other ways to improve your health. That’s great! Or, as my grandfather would say, “there’s nothing wrong with that” — his highest possible praise.
In fact, few medical treatments rival the massive health benefits of regular exercise. But how do you decide which type of exercise is best for you? Well, you could get advice from your doctor or a personal trainer. You might read books on fitness or sample exercise classes. It turns out, though, that many people are simply scrolling through tons of engaging “fitspirational” posts on social media. If you do that regularly — more often, say, than taking a brisk walk — a new study suggests you should rethink that strategy.
What exactly is fitspiration?
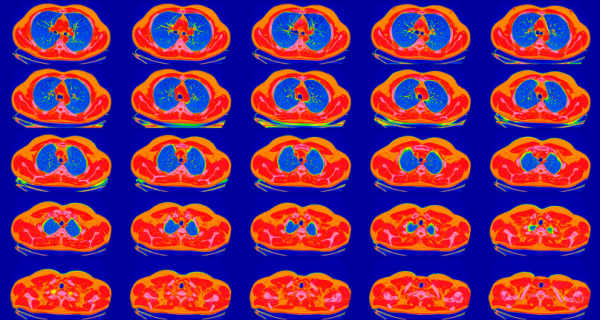
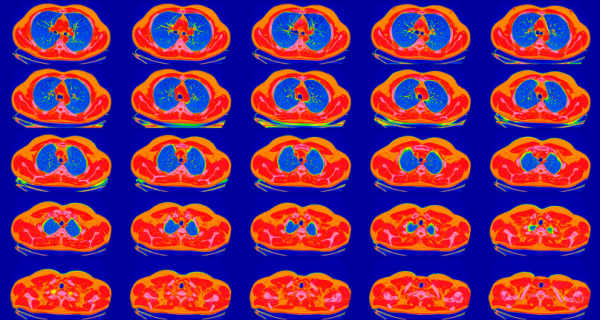
Fitspiration describes social media posts intended to inspire physical fitness and promote health. You can find fitspirational posts on TikTok, Instagram, Facebook, and other popular social media sites. Typically, they feature glossy photos and videos packaged with exercise and diet recommendations, accompanied by encouraging messages and quotes.
On Instagram alone, a search for #fitspiration (or related hashtags such as #fitspo) currently lists nearly 100 million posts. Most of them display images of attractive, lean, and fit women as they exercise and talk about fitness and optimizing health.
What’s the problem with fitspiration?
The potential benefits of a pro-fitness message reaching millions of people are obvious. But the message has to be credible and valid. And, importantly, posts should not convey inaccurate, unhelpful, or even harmful information. That’s where the problems start.
Clearly, social media posts about fitness can have positive effects, according to some research, especially when focused on realistic exercise goals rather than appearance. However, fitspirational posts may have downsides for viewers, including
- increased body dissatisfaction
- negative mood
- decreased perception of attractiveness
- embracing thinness as the ideal
- a limited range of diverse body shapes and types, suggesting that beauty is defined by being ultra-fit and thin
- a focus on appearance rather than function and capability.
A study of #fitspiration: Do these social media posts actually inspire fitness?
A recent study assesses the quality of content with fitspiration hashtags posted by Instagram influencers. The results were disappointing, though not surprising.
The authors identified 100 Instagram accounts of the most popular fitspiration influencers. Each of these accounts’ last 15 posts was analyzed. Posts were not considered credible if they
- displayed nudity or revealing clothing, such as wearing a bikini at the gym
- sexualized the person exercising, such as focusing on a woman’s breasts
- included images of extreme body types, such as people who are severely underweight or extremely muscular
- conveyed messages encouraging thinness or other negative messages rather than emphasizing health
- contained fitness information in three or fewer posts out of 15.
Here’s what the researchers found:
- 26% portrayed sexualized images
- 22% posted nudity or images of people exercising in revealing clothing not appropriate for exercise
- 15% featured people with extreme body types
- 41% posted fitness-related content in three or fewer posts.
A quarter of these accounts failed the credibility test on more than one of these criteria. Even among the accounts considered credible, only half were posted by people with credentials related to fitness or health, such as certification as a physical therapist or personal trainer.
While this study did not examine whether the posts had an actual impact on fitness outcomes, the findings raise questions about the quality of fitspiration content.
What does this mean for you?
If you’re looking for fitness-related health content, seek out the best information you can. Be skeptical of any sources lacking credentials related to fitness. Be especially wary of posts selling a product or service.
The authors of this study established certain criteria for fitness-related content they reviewed. You could apply this to posts you see online.
The bottom line
It should be no surprise to find that when it comes to health information, social media may not always be the best place to start.
While taking steps to improve your health is commendable — truly, there’s nothing wrong with that! — getting motivated to be more physically active is just a start. Information you rely on to improve your physical fitness shouldn’t just look appealing. It should be well-vetted for safety and backed by solid evidence that it can actually improve your health.
Here’s to better fitness in the New Year!
About the Author
Robert H. Shmerling, MD, Senior Faculty Editor, Harvard Health Publishing; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Robert H. Shmerling is the former clinical chief of the division of rheumatology at Beth Israel Deaconess Medical Center (BIDMC), and is a current member of the corresponding faculty in medicine at Harvard Medical School. … See Full Bio View all posts by Robert H. Shmerling, MD